Your cart
There are no more items in your cart
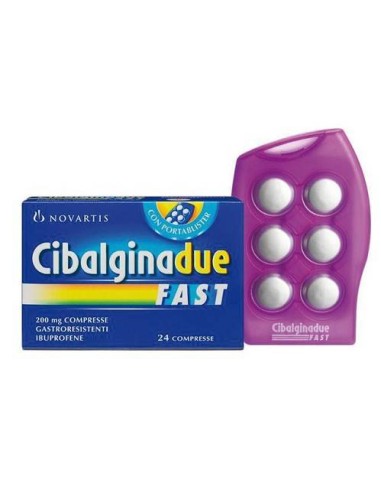
Anti-inflammatory Cibalgina two fast 24cpr 200mg Cibalgina
CIBALGINA DUE FAST 200 MG COMPRESENTATIONS
active ingredients
One tablet contains - Active ingredient: ibuprofen 200 mg. For the full list of excipients, see paragraph 6.1.Excellent
Etilcellulose; cellulose acetate phthalate; corn starch; microcrystalline cellulose; saccharin; sodium croscarmellosa; strawberry aroma; fumaric acid; silicon dioxide; magnesium stearate; calcium dibasic anidro phosphate.Therapeutic indications
Pain from various origins and nature (headache, toothache, neuralgia, osteo-articolar and muscle pain, menstrual pain). Helpful in the symptomatic treatment of feverish and flu states.Contraindications
Do not administer under 12 years of age. Hypersensitivity to the active ingredient or any of the excipients listed in paragraph 6.1. Subjects with hypersensitivity to acetylsalicylic acid or other analgesics, antipyretics, non-steroid anti-inflammatory drugs (NSAID), in particular when hypersensitivity is associated with nasal polyposes, asthma and angioedema, and occurs with bronchospasm, urticaria or acute rhinitis (see also paragraph 4.4). Severe or active peptic ulcer. History of gastrointestinal hemorrhage or perforation related to previous active treatments or history of hemorrhage/recurring peptic ulcer (two or more separate episodes of proven ulceration or bleeding). Hemopoietic disorders of unknown origin. Hemorrhage cerebrovascular or other. Hepatic or severe kidney failure. Severe heart failure (IV class NYHA). Third quarter of pregnancy (see paragraph 4.6).Population
Population: Adults, seniors and teenagers over 12 years: 1-2 gastro-resistant tablets 2-3 times daily. Do not exceed the dose of 6 tablets (1200 mg) within 24 hours. Do not exceed the recommended doses; in particular, elderly patients should comply with the above minimum dosages. In case the use of the medicine is necessary for more than 3 days in adolescents, or in case of worsening of the symptomatology the doctor must be consulted. Undesirable effects can be minimized with the use of the minimum effective dose for the shortest possible treatment duration needed to control symptoms (see paragraph 4.4). Method of administration: the tablets dissolve quickly in the mouth without leaving any unpleasant taste, pressing them with the tongue against the palate. Follow a glass of water if necessary. It is advisable to take the medicine during or after meals, especially in the presence of gastric disorders. Use only for short periods of treatment. After 2-3 days of treatment without appreciable results consult your doctor.Conservation
This medicine does not require any special condition of conservation.Warnings
General information Undesirable effects can be minimized with the use of the lowest effective dose for the shortest possible duration of treatment needed to control symptoms (see below paragraphs on gastrointestinal and cardiovascular risks). The use of Cibalgina Due Fast, as of any drug inhibitor of the synthesis of prostaglandins and cyclo-oxygenase, is not recommended in women who intend to start a pregnancy. The administration of Cibalgina Due Fast should be suspended in women who have fertility problems or who are subject to fertility surveys. In dehydrated adolescents there is a risk of alteration of kidney function. Cibalgina Two Fast contains sodium Cibalgina Due Fast contains less than 1 mmol (23 mg) of sodium per tablet, i.e. essentially ‘without sodium’. Seniors : elderly patients have an increase in the frequency of adverse reactions to NSAIDs, especially bleeding and gastrointestinal perforations, which can be fatal (see paragraph 4.2). Like other NSAIDs, ibuprofen can mask signs and symptoms of infection due to its pharmacodynamic properties. The use of Cibalgina Due Fast must be avoided in conjunction with other NSAIDs, including selective COX-2 inhibitors (see paragraph 4.5), as this entails an increase in the risk of adverse effects. Gastrointestinal effects Gastrointestinal hemorrhage, ulceration or perforation, which may be fatal, have been reported with all NSAIDs, including ibuprofen, and may occur at any time during treatment, with or without warning symptoms or previous history of serious gastrointestinal events. Patients with history of gastrointestinal toxicity, especially elderly, must report any unusual gastrointestinal symptoms (especially gastrointestinal hemorrhage) in particular in the early stages of treatment. When hemorrhage or gastrointestinal ulcer occurs in patients taking Cibalgina Due Fast treatment must be suspended. In the elderly and in patients with history of ulcer, especially if complicated by hemorrhage or perforation (see paragraph 4.3), the risk of gastrointestinal hemorrhage, ulceration or perforation is higher with increased doses of NSAID. These patients must begin treatment with the lowest dose available. For these patients and also for patients taking at the same time low doses of acetylsalicylic acid or other drugs that may increase the risk of gastrointestinal events should be taken into account a concomitant therapy with gastroprotector agents (misoprostol or protonic pump inhibitors) (see below and paragraph 4.5). Cautisus should be lent to patients taking concomitant medications that could increase the risk of ulceration or bleeding, such as systemic corticosteroids, anticoagulants such as warfarin, selective serotonin reuptake inhibitors or anti-aggregating agents such as acetilsalicylic acid (see paragraph 4.5). When hemorrhage or gastro-intestinal ulcer occurs in patients taking Cibalgina Due Fast, treatment should be suspended. NSAIDs should be given with caution in patients with a history of gastrointestinal disease ( ulcerative colitis, Crohn's disease) since such conditions can be exacerbated (see section 4.8). Hepatitis effects When ibuprofen is prescribed to patients with altered liver function, strict medical surveillance is required, as their condition may be exacerbated. As with other NSAIDs, including ibuprofen, the values of one or more liver enzymes can increase. In case the ibuprofen is prescribed for a prolonged period of time, regular monitoring of liver function as a precautionary measure is indicated. If you see persistence or worsening of altered liver function values, if signs or symptoms are developed compatible with the development of liver disease or if other manifestations occur (e.g. eosinophilia, rash), treatment with ibuprofen should be suspended. Using ibuprofen can develop hepatitis without prodromic symptoms. Ibuprofen is contraindicated in case of severe liver failure (see paragraph 4.3). When ibuprofen is administered in patients with liver porphyria, attention is required as the drug may trigger an attack. Renal effects Since fluid retention and edema have been reported in association with NSAID therapy, including ibuprofen, particular caution is required in patients with impaired heart and kidney function, history of hypertension, elderly, patients who receive a concomitant treatment with diuretics or drugs that can significantly impact kidney function, and in those patients with substantial depletion of extracellular volume from any cause, for example before or after surgery. In such cases when ibuprofen is administered, monitoring of kidney function is recommended as a precautionary measure. The termination of treatment is usually followed by a return to the pre-treatment state. Ibuprofen is contraindicated in case of severe kidney or heart failure (see paragraph 4.3). Skin effects Severe skin reactions some of which fatal, including exfoliative dermatitis, Stevens-Johnson syndrome and epidermal toxic necrolysis, have been reported very rarely in association with the use of NSAIDs, including ibuprofen (see paragraph 4.8). In the early stages of therapy patients seem to be at higher risk: the onset of reaction occurs in most cases within the first month of treatment. Generalized acute urstolosis (PEAG) was reported in relation to medicines containing ibuprofen. Cibalgina Due Fast must be interrupted to the first appearance of skin rash, mucosa lesions or any other sign of hypersensitivity. Cardiovascular and cerebrovascular effects Clinical studies suggest that the use of ibuprofen, especially at high doses (2400 mg/die), may be associated with a modest increase in the risk of arterial thrombotic events (e.g. myocardial infarction or stroke). In general, epidemiological studies do not suggest that low doses of ibuprofen (e.g. ≤ 1200 mg/die) are associated with an increase in the risk of arterial thrombotic events. Patients with uncontrolled hypertension, congestive heart failure (II-III class NYHA), proven ischemic cardiopathy, peripheral arterial disease and/or cerebrovascular disease should be treated with ibuprofen only after careful consideration and should avoid high doses (2400 mg/die). Careful consideration should be exercised even before starting long-term treatment patients with risk factors for cardiovascular events (e.g. hypertension, hyperlipidemia, diabetes mellitus, cigarette smoking habit), especially if high doses (2400 mg/die) are required of ibuprofen. Before starting treatment in patients with positive anamnesiums for hypertension and/or heart failure, caution is required, as retention of fluids, hypertension and edema were found in association with NSAIDs. Pre-existing respiratory diseases In patients with asthma, seasonal allergic rhinitis, nasal mucosa edema (e.g. nasal polyposi), chronic obstructive pulmonary disease or chronic respiratory tract infections (especially if related to symptoms similar to those of allergic rhinitis), reactions to NSAIDs such as as asthma exacerbation, Quincke edema or hives are more frequent than in other patients. Special caution is recommended in these patients (emergency patients). Ibuprofen is contraindicated in subjects with hypersensitivity to acetylsalicylic acid or other analgesics, antipyretics, non-steroidal anti-inflammatory drugs (NSAID), especially when hypersensitivity is associated with nasal and asthma polypoxes (see paragraph 4.3). Bronchospasm can be exacerbated in patients suffering from or with a previous history of asthma, allergic diseases or nasal polyps. Lupus Eritematoso Sistemico (LES) and mixed connective tissue disease In patients with LES and mixed connective tissue disorders there may be an increased risk of aseptic meningitis (see below and paragraph 4.8). Synthetic Meningitis In patients treated with ibuprofen, a septic meningitis was rarely observed. Although it is likely that this occurs more likely in patients suffering from Lupus Eritematoso Sistemico and related diseases of connective tissue, it has also been reported in subjects without a basic chronic disease.Interactions
Use caution in patients treated with any of the following medicines, since in some patients interactions have been reported. Acetylsalicylic acid Concurrent administration of ibuprofen and acetylsalicylic acid is not generally recommended due to the potential increase in unwanted effects. Experimental data suggests that ibuprofen can competitively inhibit the effect of acetylsalicylic acid at low doses on platelet aggregation when the two drugs are administered simultaneously. Although there are uncertainties regarding the extrapolation of this data to the clinical situation, the possibility that regular use, long-term of ibuprofen, can reduce the cardioprotective effect of acetylsalicylic acid at low doses. No significant clinical effect is considered likely due to occasional use of ibuprofen (see paragraph 5.1). Other NSAIDs included selective COX-2 inhibitors: avoid the concomitant use of two or more NSAIDs as this entails an increase in the risk of adverse effects (see paragraph 4.4). Litio : hybuprofen can increase plasma concentrations of lithium, for reduced elimination of the latter. It is therefore recommended to monitor the serum levels of lithium. Digoxin : ibuprofen, like other NSAIDs, can exacerbate heart failure, reduce glomerular filtration speed (VFG) and increase plasma concentrations of digoxin. It is therefore recommended to monitor the serum levels of digoxin. Diuretics and antihypertensive agents : like other NSAIDs, the concomitant use of ibuprofen with diuretics or antihypertensive agents (e.g. beta-blockers, ACE-inhibitionrs, angiotensin antagonists II) can cause a reduction of their antihypertensive effect. Therefore, the combination must be administered with caution and patients, especially elderly, must be subjected to periodic monitoring of blood pressure. Patients should be properly hydrated and should be taken into account the monitoring of kidney function after the start of concomitant therapy and periodically afterwards, especially for diuretics and ACE inhibitors, due to increased risk of nephrotoxicity. Concurrent treatment with potassium-saving diuretics can be associated with increased potassium serum levels, which therefore must be monitored frequently (see paragraph 4.4). Courtesy : concurrent administration of ibuprofen and corticosteroid can increase the risk of gastrointestinal ulceration or bleeding (see paragraph 4.4). Antiagulants : NSAIDs can increase the effects of anticoagulants, such as warfarin (see paragraph 4.4). Serotonin reuptake selective agents and inhibitors (SSRIs): increased risk of gastrointestinal bleeding (see paragraph 4.4). Sulfaniluree: nSAIDs can enhance the effect of sulfaniluree. Rare cases of hypoglycemia were reported in patients treated with sulfaniluree taking ibuprofen. It is recommended to monitor the blood glucose level in case of concurrent use with ibuprofen. Methodology: nSAIDs can reduce metotrexate clearance through tubular secretion inhibition. The administration of ibuprofen 24 hours before or after the administration of metotrexate may lead to an increase in the concentration of metotrexate and to an increase in its toxic effect. Therefore, the concomitant use of NSAIDs and high doses of metotrexate should be avoided. If concurrent administration is necessary, the patient must be carefully monitored for toxicity, especially myeloppression and gastrointestinal toxicity. Moreover, the potential risk of interactions should also be taken into account in the treatment at low doses of metotrexate ( Ciclosporine and tacrolimus: The risk of a nephrotoxic effect due to cyclosporin and tacrolimus, due to the reduction of prostaglandine synthesis in the kidney, increased from the concomitant administration of some non-steroidal anti-inflammatory drugs, including ibuprofen. Therefore, ibuprofen should be administered at lower doses than those used in patients who do not take these immunosuppressive agents and kidney function is strictly controlled. Fluoquinox antibacterial: there have been isolated cases of seizures that may have been induced by the concomitant use of fluorochinolone and NSAIDs. Fenitoine: when using phenytoin in conjunction with ibuprofen, blood levels of phenytoin can increase. The monitoring of plasma concentrations of phenytoin is therefore recommended. Colestipolo e colestiramina: when administered at the same time to ibuprofen, they can induce a delay or decrease the absorption of the latter. Therefore, it is recommended to administer ibuprofen at least 1 hour before or 4-6 hours after administration of colestipolo/colestiramine. Powerful inhibitors of CYP2C9: concurrent administration of ibuprofen with inhibitors of CYP2C9 (such as sulfinpirazone, fluconazole and voriconazole) requires caution, because it could lead to a significant increase in peak plasma concentrations and exposure to ibuprofen, due to the inhibition of ibuprofen metabolism. In a study with voriconazole and fluconazole (CYP2C9) inhibitors, an increase in exposure to the S (+)-ibuprofen approximately from 80 to 100% was highlighted. Therefore a reduction in the dose of ibuprofen should be considered when administered in conjunction with powerful CYP2C9 inhibitors, particularly when high doses of ibuprofen are administered with voriconazole or fluconazole. Zidovudina: there is an increased risk of hematological toxicity in case of simultaneous administration with NSAIDs. There are evidence of an increased risk of hematrosis and hematomas in seropositive hemophilic patients for HIV treated simultaneously with zidovudine and ibuprofen. Aminoglycosides : when administered simultaneously to ibuprofen, they can lead to a reduction in kidney function in sensitive subjects, reduced elimination of aminoglycosides and increased plasma concentrations.Effects
The most commonly observed adverse events are gastrointestinal. Peptic ulcers, perforation or gastrointestinal hemorrhage may occur, sometimes fatal, especially in the elderly (see section 4.4). Undesirable effects are mostly dose-dependent and may vary from patient to patient. In particular, the risk of gastrointestinal hemorrhage is dependent on dose and duration of treatment. After administration of Cibalgina Due Fast have been reported: nausea, vomiting, diarrhea, flatulence, constipation, dyspepsia, abdominal pain, melena, ematemesis, ulcerative stomatitis, exacerbation of colitis and Crohn's disease (see section 4.4). Less frequently gastritis were observed. In association with the treatment with the NSAIDs were reported edema, hypertension and heart failure. Clinical studies suggest that the use of ibuprofen, especially at high doses (2400 mg/die), may be associated with a modest increase in the risk of arterial thrombotic events (e.g. myocardial infarction or stroke) (see paragraph 4.4). Adverse reactions are listed below, depending on the classification for organ and frequency systems. The frequencies are defined as: very common (≥ 1/10); common (≥1/100, not common (≥1/1.000, rare (≥ 1/10.000; very rare (not known (frequency cannot be defined on the basis of available data).| Infections and infestations | ||
| Very rare: | Deterioration of inflammations associated with infection (e.g. development of necrotizing fascites) described in coincidence with the use of non-steroidal anti-inflammatory drugs. 1 | |
| Emolinfopoietic system pathologies | ||
| Very rare: | Trombocytopenia, anemia, leucopenia, pancitopenia, agranulocytosis2. | |
| Immune system pathologies | ||
| Not common: | Reactions of hypersensitivity, including rash, hives, itching, and asthmatic attacks. | |
| Very rare: | Anaphylactic reaction, angioedema. | |
| Psychiatric disorders | ||
| Notable: | Psychic reactions, depression | |
| Diseases of the nervous system | ||
| City: | Sleep | |
| Not common: | Headache, dizziness, insomnia, agitation, irritability, fatigue. | |
| Very rare: | Aseptic Meningitis3 (see paragraph 4.4) | |
| Pathologies of the eye | ||
| Notable | Visual disturbances | |
| Ear and labyrinth pathologies | ||
| Rare: | Tinnitus, compromise of hearing. | |
| Heart disease | ||
| Notable | Palpitations, edema, heart failure, myocardial infarction | |
| Vascular diseases | ||
| Notable: | Hypertension | |
| Gastrointestinal diseases | ||
| City: | Despepsia, abdominal pain, nausea, vomiting. | |
| Rare: | Peptic ulcer, perforation or gastrointestinal hemorrhage, ulcerative stomatitis, gastritis. Worse than Crohn's colitis and disease (see paragraph 4.4). | |
| Notable: | Esophagitis, pancreatis, obstruction of the small intestine for formation of a thin wall similar to a diaphragm (intestinal diaphragm disease), flatulence, diarrhea, constipation. | |
| Hepatobiliary diseases | ||
| Very rare: | Alteration of liver function tests, alteration of liver function, jaundice, hepatitis. Epathetic damage4 | |
| Pathologies of skin and subcutaneous tissue | ||
| Not common: | Skin rash | |
| Very rare: | Stevens-Johnson's syndrome, toxic epidermal necrolysis, bully dermatitis. | |
| Notable: | Reaction from drug with heosinophilia and systemic symptoms ( DRESS syndrome), generalized acute hexantholysis (PEAG), photosensitivity reactions. | |
| Renal diseases | ||
| Rare: | Renal insufficiency, renal tissue damage (papal necrosis4), increased serum concentration of uric acid. | |
| Notable: | Formation of edema, especially in patients with arterial hypertension or kidney failure, nephrotic syndrome, interstitial nephritis that can be accompanied by acute kidney failure. | |
Overdosing
Toxicity Signs and symptoms of toxicity were generally not observed at doses less than 100 mg/kg in children or adults. However, in some cases you may need a support treatment. It has been observed that children manifest signs and symptoms of toxicity after ingestion of ibuprofen at doses of 400 mg/kg or greater. Synonyms Most patients who have ingested significant quantities of ibuprofen will manifest symptoms within 4-6 hours. The most commonly reported overdose symptoms include: nausea, vomiting (with possible presence of traces of blood), abdominal pain, lethargy and drowsiness, confusion, nistagm. The effects on the central nervous system (SNC) include headaches, tinnitus, dizziness, convulsions (even myoclonic seizures in children), dizziness and loss of consciousness. Hypothermia, kidney effects, gastrointestinal bleeding, coma, apnea, cyanosis, diarrhea and depression of the SNC and respiratory system have rarely been reported. Disorientation, state of excitement, fainting and cardiovascular toxicity including hypotension, bradycardia and tachycardia, chest pain, palpitations, weakness, hematuria, feeling of cold to the body and occurrence of respiratory problems. Asthmatic patients can exacerbate the condition. In cases of significant overdose are possible kidney failure and liver damage. In cases of severe poisoning, it is possible that metabolic acidosis occurs and that protrombine/INR time may be prolonged, probably due to interference with the circulating factors of coagulation. Treatment There is no specific antidote for overdosing ibuprofen. In case of overdose, a symptomatic and support treatment is therefore indicated. Particular attention is given to the control of blood pressure, acid-base balance and gastrointestinal bleeding. An adequate diuresis must be ensured and renal and hepatic functions must be closely monitored. The patient must remain under observation for at least four hours after ingestion of a potentially toxic drug. Any occurrence of frequent or prolonged seizures must be treated with intravenous diazepam. Give bronchodilators for asthma. Other support measures may be required in relation to the patient's clinical conditions. For more information, contact the local anti-veleni center.Pregnancy
Inhibition of prostaglandin synthesis may adversely affect pregnancy and/or embryo/fetal development. Results of epidemiological studies suggest an increased risk of abortion and cardiac malformation and gastroschisis after the use of an inhibitor of prostaglandin synthesis in the early stages of pregnancy. The absolute risk of heart failure increased from less than 1% to about 1.5%. It has been estimated that the risk increases with dose and duration of therapy. In animals, the administration of prostaglandin synthesis inhibitors showed an increase in the loss of pre- and post-plant and embryo-fetal mortality. In addition, an increase in the incidence of various malformations, including cardiovascular disorders, was reported in animals that had been given prostaglandin synthesis inhibitors during the organogenetic period. During the first and second trimester of pregnancy, Cibalgina Due Fast should not be administered if not in strictly necessary cases. If Cibalgina Due Fast is used by a woman waiting for conception, or during the first and second trimester of pregnancy, the dose and duration of treatment must be kept as low as possible. During the third trimester of pregnancy, all prostaglandin synthesis inhibitors can exhibit: - fetus a: - cardiopulmonary toxicity (with premature closure of arterial duct and pulmonary hypertension); - kidney dysfunction, which can progress in kidney failure with oligo-idroamnios; - the mother and the newborn, at the end of pregnancy, to: - possible prolongation of the time of bleeding, and anti-aggregating effect that can also be necessary at very low doses; - inhibition of uterine contractions resulting in delay or extension of labor. Consequently, Cibalgina Due Fast is contraindicated during the third trimester of pregnancy.Food
Hybuprofen passes into breast milk in small quantities. Although no undesirable effects in the infant are known today, caution should be given when ibuprofen is given to a nursing woman.Fertility
There are evidence that drugs that inhibit cycloxygenase/prostaglandin synthesis can cause a reduction in female fertility due to ovulation. This event is however reversible with the suspension of treatment. Women who are planning a pregnancy should pay attention in case of hiring ibuprofen.Source: Farmadati
- Deductible product
- Yes
029500055
190 Items
New
No reviews